Tuberculosis
Tuberculosis (TB)
What It Is, Where to Get Tested, and What to Do if You Have It
Tuberculosis (TB) is a serious disease that affects people all over the world. TB used to be one of the leading causes of death in the United States, but not anymore. In most cases, tuberculosis is preventable, treatable, and curable.
TB is an airborne bacterium called Mycobacterium tuberculosis. TB usually affects the lungs, but it sometimes harms other parts of the body, like the brain, kidneys, lymph nodes, or spine. Common symptoms of TB include weakness, fever, weight loss, fatigue, night sweats, chest pain, and a cough (sometimes a bloody cough) that won’t go away. Thanks to the knowledge and medications we have today, TB can be cured. If left untreated, TB disease can lead to disability and death.
Although the number of TB cases in the United States has been dropping over the past 20 years, San Mateo County still experiences a significant number of TB cases each year.
To see how TB affects San Mateo County, take a look at our latest 2024 Annual TB Report, and then join us in the fight to prevent and cure TB!
How can I tell if I have TB?
The best way to know if you have TB is to get a TB test.
There are two kinds of tests: a skin test and a blood test. Either test can tell if you’ve been infected by the TB bacteria.
If you’ve been infected, you might need other follow-up tests to tell whether you have active TB disease.
Symptoms of TB depend on which part of the body is affected.
Most people with TB disease have a cough that won’t go away, feel weak or sick, lose weight, have fever, and have night sweats. If you have any of these symptoms, contact your doctor right away.
Where can I get tested for TB in San Mateo County?
- You can ask your doctor for a TB skin test or blood test
- You can visit one of the San Mateo County TB Testing Clinics that offer TB skin tests or TB blood tests
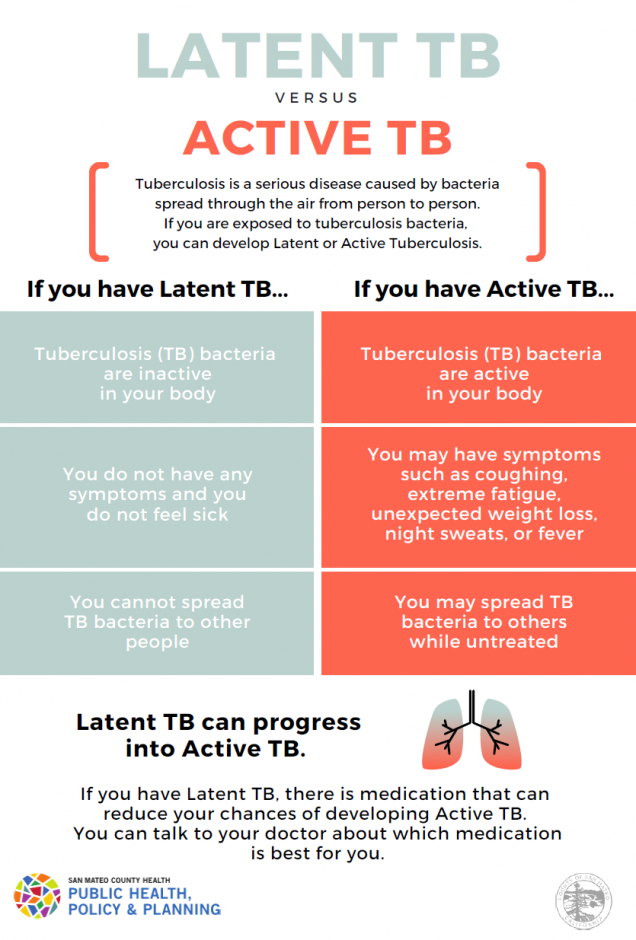
What’s the difference between active TB disease and latent TB infection (LTBI)?
Active TB disease occurs when TB bacteria are active in a person’s body in large numbers. People with active TB disease usually feel sick and have one or more symptoms of TB disease. They may be infectious, which means they can pass the TB bacteria on to others. If it’s not treated, TB disease can cause serious disability and even death.
Latent Tuberculosis Infection (LTBI) is caused by the same bacteria, but it’s less serious. People with LTBI are not sick because they have fewer of the bacteria in their body, and the bacteria are latent (inactive). People with LTBI are not contagious. That means they cannot spread the bacteria to others. People with TB infection can end up developing TB disease in the future, especially if they are in one of the high-risk groups. People with TB infection can take medicine to keep from developing TB disease.
This chart explains the differences between TB disease and TB infection. TB Latente vs. TB Activa Latent TB laban sa Aktibong TB
Who is at-risk for developing active TB?
If you have latent TB infection, you may never develop active TB disease. The risk of developing TB disease is higher if you:
- Have HIV infection
- Have been infected with TB bacteria recently (in the last 2 years)
- Have other health problems, like diabetes, that make it hard for your body to fight disease
- Take medications that suppress your immune system
- Use alcohol or misuse drugs
- Don’t eat enough healthy food
- Smoke cigarettes
- Were not treated correctly for LTBI in the past
- Are a child younger than 5
Treating Latent TB Infection (LTBI)
To reduce the risk of active tuberculosis from developing, treatment for LTBI is recommended.
Of the LTBI treatments available, the preferred methods are the short-course treatment options: either rifampin daily for 4 months or isoniazid plus rifapentine weekly for 12 weeks.
- If a rifamycin-based regimen is not an option (due to drug interactions or intolerance), use isoniazid daily for 9 months
The California Department of Public Health – TB Branch has more information regarding LTBI treatments. Also, see these treatment fact sheets:
While you’re taking medication for latent TB infection (LTBI), you should check in with your healthcare provider as scheduled to make sure your treatment is going well.
TB medicines are usually safe, although some people may have side effects. If you think you are having any side effects to your TB medicine, call or see your doctor right away.
If I have active TB, how can I get better?
To get better, you should follow these important steps:
- You need to see a doctor and take special medication for active TB disease.
- TB bacteria are strong and live a long time. You will feel better a few weeks after you start to take the TB medication. Even if you feel better, you must keep taking TB medication until your doctor has ended your treatment.
- It’s important to work with your public health nurse and see your doctor regularly until your TB treatment is finished. The doctor will do follow-up tests to make sure you’re getting better, to ask if you have any problems with your medicines, and to answer your questions.
Many people take TB medication every day without any problems, but there are a few things you should watch for:
- Poor appetite, losing weight, or feeling tired for no reason
- Nausea or vomiting. If you have nausea when you begin taking your pills, try eating a little food with your pill.
- Pain in your abdomen
- Dark urine (the color of strong tea)
- Yellow skin or eyes
- Skin rash or itching
- Numbness or tingling in your hands or feet
- Coughing for more than three weeks
- Sweating at night
- Fever for longer than 3 days
If you have any of these problems, call your doctor right away – don’t wait for your next appointment.
Other important things to remember:
- Drinking alcohol while you take TB medicine can hurt your liver. Don’t drink beer, wine, or liquor until you completely finish your TB treatment.
- Be sure to tell your doctor if you are taking any other medicine or if you think you may be pregnant.
Immigration Clearance
Civil Surgeon Patients (Completing I-693 Form for Immigration Status Adjustment)
Persons undergoing immigration status adjustment undergo a medical exam as part of immigration screening requirements. The exam must be done by a U.S. Citizenship and Immigration Services (USCIS) authorized doctor (referred to as a civil surgeon). USCIS designates civil surgeons to perform the medical exam. To read more information or to find a civil surgeon, please visit the USCIS website.
The CDC Division of Global Migration and Quarantine requires that civil surgeons report tuberculosis (TB) screening outcomes that result in Latent TB Infection (LTBI) diagnosis to local public health departments. If you live in San Mateo County and are found to have LTBI by a civil surgeon, someone from San Mateo County Public Health will be reaching out to you to provide LTBI education, ensure proper screening, connect you to services, and/or monitor treatment. To reduce the risk of active tuberculosis from developing, treatment for LTBI is recommended.
Please reach out to 650-573-2346 if you have any questions. If you are a provider, please visit our Provider Website.
Clearance for Newly Arriving Immigrants
Local health departments are notified of newly arriving immigrants/refugees with findings related to tuberculosis. While processing tuberculosis immigration clearance, San Mateo County is notified of people who need further evaluation. If you are a new arriver and have findings related to tuberculosis, someone from San Mateo County Public Health Department will reach out to you to ensure proper evaluation, connect you to services, and/or monitor treatment.
For assistance accessing health insurance, please contact the Health Coverage Unit at (650) 616-2002.
FAQs
I’ve had a BCG vaccine. Doesn’t that protect me from TB?
The BCG vaccine (a TB vaccine) can help keep young children from getting serious complications of TB. However, this protection goes away as people get older. People who were vaccinated with BCG can still get latent TB (inactive) infection and active TB disease.
If you had the BCG vaccine and you’re offered a choice between a TB blood test and a TB skin test, it’s a good idea to choose the blood test. This is because the TB blood test is not affected by the BCG vaccine. This means that your TB blood test will be “positive” only if you have TB germs in your body.
If you’ve had the BCG vaccine and you don’t have the choice to get a TB blood test, you should still have the TB skin test.
I have no symptoms – do I still need to be screened?
If you were found to be exposed to someone with active TB disease, you should be screened regardless of if you have symptoms because there is still a chance that you have active TB disease or latent TB infection (LTBI). The only way to tell if you have either is to be tested. For more information, check out the above sections regarding testing and Active TB disease vs. Latent TB infection.
Where can I get a TB test?
- You can ask your doctor for a TB skin test or blood test
- You can visit one of the San Mateo County TB Testing Clinics that offer TB skin tests or blood tests
- If you have been notified about being in contact with someone who has active TB, the County Health System can help you get tested for TB, even if you don’t have a regular doctor
How is TB spread?
- TB bacteria are spread from person to person through the air.
- TB bacteria get into the air when a person with Active TB disease of the lungs or throat coughs, sneezes, laughs, or sings.
- TB is NOT spread by touching or sharing dishes.
Do staff and children in school or childcare need to be tested for TB?
- California Tuberculosis Screening Guidelines for Child Care Centers and Schools
- In San Mateo County, TB screening requirements for students in Kindergarten through 12th Grade are determined by the school district. Please contact your school district office for more information.
Here are 3 things you can do to reduce TB in San Mateo County
- Learn the symptoms of TB disease
- If you have symptoms (or are close to someone with symptoms), ask your healthcare provider about TB testing
- If you’re being treated for TB, take all your medicine, exactly as your doctor prescribed it. Early treatment with antibiotics cures TB disease, so it’s very important to follow your doctor’s instructions and take all your medicine.
Resources to learn more about TB
- Sputum Collection Instructions:
- Home Isolation Instructions:
- CDC Questions and Answers about TB
- TB General Information
- Basic TB Facts Podcast
- TB Data and Stats